Pneumonia, a lung infection that can range from mild to life-threatening, is a significant health challenge, especially in healthcare settings. Nurses play a crucial role in caring for patients with pneumonia, and their approach has evolved significantly over the years. This post aims to shed light on the basics of pneumonia and how nursing care for this condition has transformed from traditional practices to modern, evidence-based approaches.
Overview of Pneumonia and Its Relevance in Healthcare
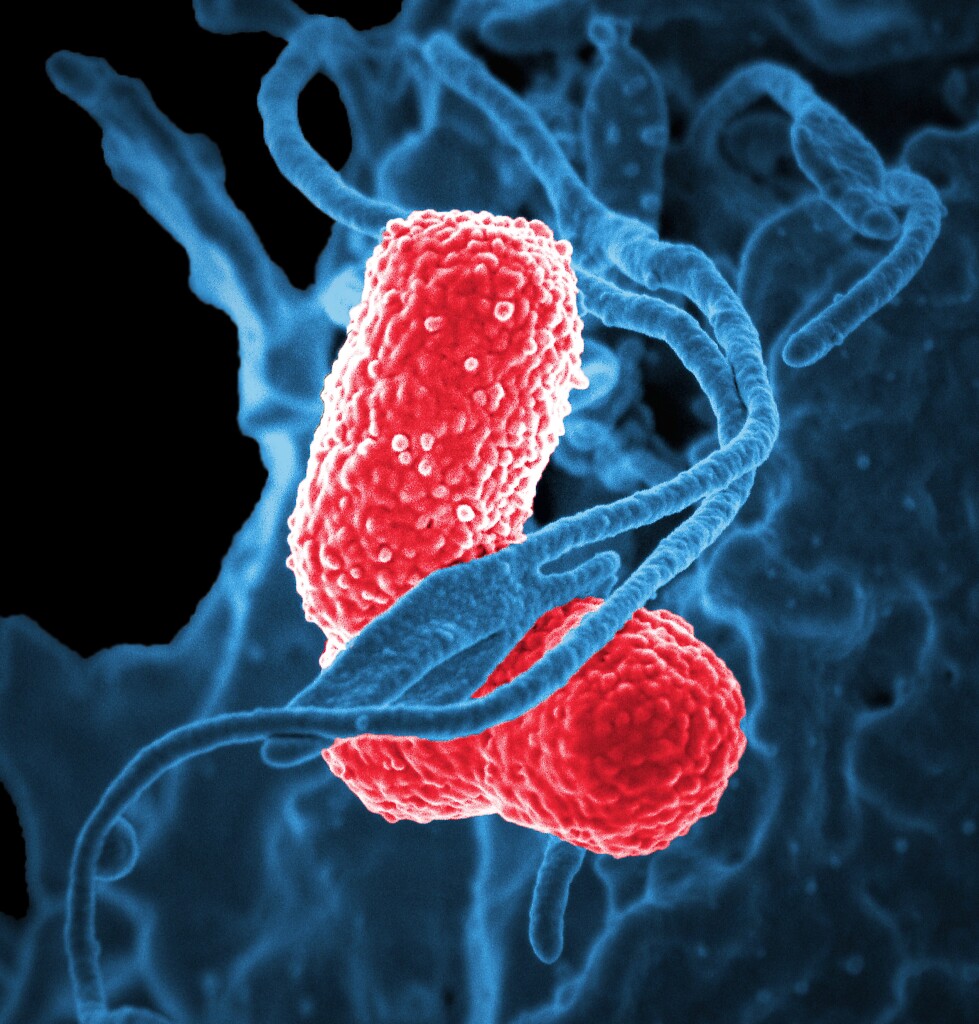
Pneumonia is an infection that inflames the air sacs in one or both lungs. These air sacs may fill with fluid or pus, causing symptoms such as cough, fever, chills, and difficulty breathing. Various organisms, including bacteria, viruses, and fungi, can cause pneumonia. The condition can vary in severity, being most serious for infants, older adults, and people with health problems or weakened immune systems.
In healthcare, pneumonia is a common ailment and a significant cause of hospitalization. It’s especially prevalent in hospital and long-term care settings, where patients are more vulnerable. This high prevalence makes understanding pneumonia crucial for nursing professionals, as they are often the first line of defense in identifying and managing this condition.
Evolution of Pneumonia Nursing Care: From Traditional to Modern Approaches
Traditional Nursing Care for Pneumonia In the past, nursing care for pneumonia was primarily supportive, focusing on bed rest, providing nutrition, and managing symptoms. Nurses relied heavily on physician guidance and less on evidence-based practices.
Transition to Modern Nursing Care With advances in medical knowledge and technology, nursing care for pneumonia has become more dynamic and evidence-based. Nurses now play a pivotal role in the diagnosis, treatment, and prevention of pneumonia. This shift has been fueled by better diagnostic tools, a greater understanding of the disease process, and more effective treatments.
Current Best Practices in Pneumonia Nursing Care Today, nursing care for pneumonia involves a comprehensive approach:
Assessment and Monitoring: Regular monitoring of vital signs, oxygen levels, and patient symptoms.
Medication Management: Administering antibiotics, antivirals, or antifungals as prescribed, along with medications for symptom relief.
Patient Education: Instructing patients about medication adherence, hygiene practices, and breathing exercises.
Prevention: Implementing measures to prevent the spread of infection, like vaccination and infection control practices.
Community-Acquired Pneumonia (CAP) in Critical Care

Community-Acquired Pneumonia (CAP) is a major health concern globally and is recognized as the leading infectious disease cause of mortality across all age groups. It poses unique challenges in critical care due to its high morbidity and mortality rates. Severe CAP often leads to long-term health issues like reduced lung function and cognitive abilities. Effective management of CAP in critically ill patients relies on timely diagnosis and appropriate antimicrobial treatment, which are central to improving patient survival rates and outcomes.
Hospital-Acquired Pneumonia (HAP) and Ventilator-Associated Pneumonia (VAP): Incidence and Impact Hospital-Acquired Pneumonia (HAP) occurs in patients hospitalized for more than 48 hours and is a significant contributor to nosocomial infections. It is estimated to have an incidence of five to ten cases per 1000 hospital admissions globally. A critical subset of HAP is Ventilator-Associated Pneumonia (VAP), affecting 10-25% of patients on mechanical ventilation. VAP is especially prevalent in the initial days of mechanical ventilation. The impact of these conditions is profound, with mortality rates varying significantly and influenced by several factors. Recent prevention strategies have led to a decrease in incidence and mortality, but challenges remain in accurate diagnosis and management. The mortality rate for HAP ranges from 13-28%, with variations depending on whether it occurs in the ward or ICU, and whether it involves ventilation
Severe Community-Acquired Pneumonia (SCAP)
SCAP is a significant form of pneumonia that requires immediate and effective treatment, often in an intensive care setting. The early identification of SCAP is vital for several reasons:
Mortality and Morbidity Risk: Patients with SCAP are at a higher risk of mortality and morbidity. This risk is compounded by factors like age, comorbidities, and the severity of the pneumonia.
Scoring Systems: Tools like the Infectious Disease Society of America/American Thoracic Society (IDSA/ATS) guidelines provide criteria for identifying severe CAP. These criteria include respiratory rate, oxygenation levels, blood pressure, and mental status. Scoring systems help in assessing the severity and guiding the decision for ICU admission.
Treatment Challenges: The treatment of SCAP involves a combination of antimicrobial therapy and supportive care. The choice of antibiotics is guided by local epidemiology and the patient’s clinical condition. Early and appropriate antibiotic therapy is crucial for improving outcomes.
Hospital-Acquired Pneumonia (HAP) and Ventilator-Associated Pneumonia (VAP)

HAP and VAP represent significant challenges in the hospital setting, particularly in ICUs:
Incidence and Impact: HAP is one of the most common hospital-acquired infections, with VAP affecting a substantial proportion of patients on mechanical ventilation. These conditions are associated with increased hospital stays, healthcare costs, and mortality.
Risk Factors: The risk of developing HAP or VAP increases with the duration of hospital stay and mechanical ventilation. Other risk factors include the patient’s underlying health condition, age, and exposure to invasive devices.
Antibiotic Resistance: A major concern in the treatment of HAP and VAP is the rise of antibiotic-resistant pathogens. This resistance complicates treatment choices and is associated with poorer outcomes. Strategies to combat this include adherence to antibiotic stewardship programs and infection control practices.
Cardiovascular Disease and Pneumonia
The relationship between CAP and cardiovascular complications is an area of growing interest and concern:
Cardiac Events Post-Pneumonia: Patients with CAP, especially those with pre-existing cardiovascular disease, are at an increased risk of cardiac events such as heart failure, arrhythmias, and acute coronary syndromes.
Pathogenesis: The interaction between pneumonia and cardiac events is complex and multifactorial. It involves direct microbial invasion, systemic inflammation, and the exacerbation of existing cardiovascular conditions. Pneumonia can induce a systemic inflammatory response, which can adversely affect cardiac function.
Long-Term Implications: The impact of CAP on cardiovascular health can extend beyond the immediate period of the infection. Studies suggest a prolonged period of elevated risk for cardiac events following a pneumonia episode
In-Depth Analysis of Nursing Care Plans for Pneumonia

Pneumonia, a significant respiratory condition, demands comprehensive nursing care. Effective nursing care plans are tailored to meet the individual needs of patients, focusing on alleviating symptoms, preventing complications, and promoting recovery. Let’s delve into the key aspects of nursing care plans for pneumonia.
Prioritizing Nursing Problems and Setting Goals
- Assessment and Identification of Key Problems:
- Respiratory Distress: Nurses must assess the patient’s respiratory status regularly, noting any signs of distress such as shortness of breath, abnormal breathing patterns, or hypoxia.
- Infection Control: Monitoring signs of infection, including fever, chills, and changes in sputum, is crucial.
- Hydration and Nutrition: Ensuring adequate hydration and nutrition is vital, as patients may have decreased appetite and fluid loss due to fever and increased respiratory rate.
- Goal Setting:
- Respiratory Stability: Goals include maintaining a clear airway, achieving normal breathing patterns, and ensuring adequate oxygenation.
- Infection Management: Reducing or eliminating signs of infection and preventing the spread of pathogens.
- Overall Well-being: Maintaining adequate nutrition, hydration, and comfort.
Intervention Strategies: Traditional vs. Contemporary Approaches
- Traditional Approaches:
- Medication Administration: Ensuring timely administration of prescribed antibiotics and other medications.
- Oxygen Therapy: Providing supplemental oxygen as needed.
- Hydration and Nutrition: Encouraging fluid intake and a balanced diet.
- Contemporary Approaches:
- Use of Technology: Utilizing advanced monitoring systems for continuous assessment of respiratory and cardiac status.
- Patient Education: Leveraging digital tools for patient education about disease management and prevention strategies.
- Holistic Care: Incorporating holistic approaches like relaxation techniques and complementary therapies to manage symptoms and reduce stress.
Nursing Interventions for Specific Types of Pneumonia
Community-Acquired Pneumonia (CAP):
Home Care Education: Educating patients and families about medication adherence, symptom monitoring, and when to seek medical attention.
Vaccination Advocacy: Promoting pneumococcal and influenza vaccinations as preventive measures.
Hospital-Acquired Pneumonia (HAP) and Ventilator-Associated Pneumonia (VAP):
Infection Control Measures: Strict adherence to hand hygiene, aseptic techniques, and isolation protocols.
Ventilator Care: Regular oral care and proper positioning to prevent aspiration and ventilator-associated complications.
Aspiration Pneumonia:

Swallowing Assessment: Working with speech therapists to assess and manage swallowing difficulties.
Positioning: Keeping the patient in an upright position during and after feeding to prevent aspiration.
Pneumocystis Pneumonia (PCP) in Immunocompromised Patients:
Close Monitoring: Vigilant monitoring for any signs of respiratory distress or infection.
Collaboration with Specialists: Coordinating care with infectious disease specialists and other healthcare providers for comprehensive management.
Antimicrobial Stewardship and Treatment Strategies
Pneumonia, especially in the ICU, affects a significant portion of critically ill patients (27%). Given this high prevalence, optimizing antimicrobial therapy while minimizing toxicities is crucial. The review article from PubMed discussed methods to optimize antimicrobial treatment in pneumonia patients. These include using procalcitonin levels, MRSA nares testing to determine the need for vancomycin therapy, and advanced PCR techniques for accurate diagnosis and treatment.
Innovations in Pharmacological Interventions
A study from Karolinska Institutet highlighted the role of interleukin-26 (IL-26) in bacterial pneumonia. IL-26, a recently discovered inflammatory mediator, is involved in the innate immune response and directly kills bacteria known to cause pneumonia. This discovery positions IL-26 as a potential new target for biological treatment, which could be crucial considering the rising issue of antibiotic resistance.
Non-Pharmacological Interventions
The COVID-19 pandemic has brought attention to the effectiveness of non-pharmacologic interventions (NPIs) like masking and physical distancing. These interventions have not only impacted COVID-19 transmission but have also led to a decrease in hospitalizations for non-COVID-19 respiratory illnesses, including pneumonia. This suggests a promising role for NPIs in the prevention of pneumonia and other respiratory infections.
Conclusion and Future Directions in Pneumonia Nursing Care
Summarizing Key Takeaways This blog post aimed to provide a comprehensive overview of pneumonia in nursing care, covering the different types of pneumonia, their epidemiology, advanced diagnostic techniques, and the latest trends in treatment. We discussed the critical role of nurses in managing Community-Acquired Pneumonia (CAP), Hospital-Acquired Pneumonia (HAP), and Ventilator-Associated Pneumonia (VAP), emphasizing the importance of accurate diagnosis and timely intervention. The evolution from traditional to modern nursing approaches reflects the advancements in medical science and the increasing complexity of patient care.
Future Prospects in Pneumonia Care and Research Looking ahead, the field of pneumonia care and research is poised for significant developments. Advancements in diagnostic technology, personalized medicine, and patient care strategies will likely transform how pneumonia is managed in healthcare settings. Nurses will continue to play a vital role in this evolution, adapting to new technologies and methodologies to provide the best possible care. Ongoing research and clinical trials promise to bring forward new insights into pneumonia treatment, further enhancing patient outcomes.
References and Further Reading
- Management of pneumonia in critically ill patients – The BMJ.
- Latest guidelines on pneumonia treatment and management from reputable health organizations.
- Research articles and studies on pneumonia types, epidemiology, and treatment strategies.
- Comprehensive reviews of advances in diagnostic technologies and treatment interventions for pneumonia.
Comprehensive List of Sources and Additional Resources
- Clinical journals and medical databases for up-to-date research on pneumonia.
- Online courses and webinars focused on the latest in pneumonia care and nursing practices.
- Medical textbooks on infectious diseases and critical care nursing for in-depth understanding.
- Health organization websites for guidelines, fact sheets, and patient education materials.
